Written By: Jessica Taylor, LPC
Site Director at The Renfrew Center of Radnor

Like any component to mental health, eating disorders included, there is often great misunderstanding. What we do know about relapse: it is common, it can sometimes be functional, and it often communicates an unmet need. It can be helpful to acknowledge that a relapse may be a part of the recovery process rather than a hiatus from it.
When there is a relapse, it is normal to experience a wide range of emotions. Often people feel shameful, guilty, frustrated, and misunderstood. It is important to recognize the emotional toll that a relapse can take. Simultaneously, it is also important to consider what these feelings are signaling to us about the process.
READ MORE: 5 Tips for Navigating Eating Disorder Relapses & Promoting Sustainable Recovery
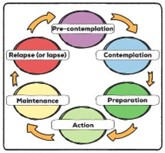
The Change Model
Taking the First Steps to Return to Treatment
That next step in recovery may mean reaching out for help. Once there is some recognition that a relapse, or lapse, has occurred, it may be time to reconnect with trusted supports. This is different for everyone. Common professional helpers often include physicians, therapists, dieticians, and other eating disorder informed healthcare providers. Outside of professional help, you may consider peer support, such as recovery groups or support groups with members who understand and can empathize, and family (chosen family included) support, like structured and shared mealtimes, to help with accountability on your path in recovery.
It may also be helpful to consider previous treatments that have helped you. Take time to reflect on what worked in your treatment planning before and revisit these strategies if applicable. Treatment is adaptable for a reason, as it is meant to fit you, and can be garnered to your current challenges. Be realistic about what you expect, from others and yourself, as you work towards small, achievable, and meaningful goals to regain your sense of confidence.
Common Barriers and How to Overcome Them
If you are fearful of reaching out for help again, there are ways to overcome those feelings. It is only natural to focus on the negative thoughts that arise during a relapse. You might tell yourself that you failed in some way, that seeking help means starting from scratch, or that others will be critical, harsh or judgmental of your need for additional support. It is less common to focus on how you manage those feelings and rewrite the narrative surrounding them. What if you shifted the focus from what is wrong with the process to what is possible? This could involve viewing your relapse as a springboard for growth and adaptation on your journey, addressing that unmet need, or choosing to see your efforts towards healing as valuable, regardless of when or how they happen.
Logistical and financial challenges can also interfere with people receiving needed support. The tasks associated with insurance options, fees, and financial arrangements can feel completely overwhelming, even for those feeling highly motivated to seek treatment. Talk to your trusted supports about the options available to make treatment fit into your life, rather than trying to make your life fit into treatment. Often, simply asking is the first step toward finding flexibility.
And then, of course, there is motivation. “What if I don’t have the energy right now to make this change?” While it is a fair reflection to ask yourself this, it is also worth asking yourself the follow-up questions: How important is this change? How confident am I that I could make this change if I wanted to? And how ready am I for this change? You may find that you are further along in your motivation than you realize.
Strengthening Support Systems
Recovery is considerably supported by three major support avenues: those in the home with you, those with lived experience, and those with expertise.
Those who live with you have some of the most readily available opportunities to support you, but their role in your recovery may not yet be clear. The first step may be to identify what non-judgmental support would look like for you in your home environment and communicate that to them. Pinpoint vulnerable times in your day when you’re more or less prone to the eating disorder behaviors and consider how you’d prefer they support you in those moments. Remind them how important it is to be patient with the process, just as you are trying to be, and that there is no ‘quick fix’ to recovery. It may also be helpful to have guidelines around appearance-based remarks, comments about food, and commentary on bodies.
The second leg of the support system is peer support. Others who have experience with eating disorders, with recovery, and with relapse, can share their stories, normalize difficult experiences, and offer encouragement on your journey. Support groups, online communities, blogs, treatment settings, and group therapies can connect you to those who will listen with a shared heartstring.
Lastly, therapists and treatment providers guide and complement the environmental support in the home and the emotional support from lived experience with the expertise and oversight necessary during times of relapse. Come prepared to be open and honest about your struggles, and you will be met with curiosity and understanding, helping you build an aligned team focused on the same goals for your recovery.
READ MORE: In Your Empowerment Era: 5 Ways to Choose Recovery
Conclusion
While it may still feel daunting to confront and unpack relapse as you return to what was once a familiar but unsustainable reality, remember that a new realm of possibility awaits you. Self-compassion and hope for the future make each effort towards healing worthwhile. There is power in progress – celebrating every victory, big or small, today – and weaving those wins into your recovery story for tomorrow.
If you’re experiencing a relapse, know that you’re not alone. Reach out to Renfrew today and explore supportive, compassionate care tailored to where you are in your recovery journey.
References:
- Berends T, van Meijel B, Nugteren W, Deen M, Danner UN, Hoek HW, van Elburg AA. Rate, timing and predictors of relapse in patients with anorexia nervosa following a relapse prevention program: a cohort study. BMC Psychiatry. 2016 Sep 8;16(1):316. doi: 10.1186/s12888-016-1019-y. PMID: 27608679; PMCID: PMC5017136.
- Khalsa SS, Portnoff LC, McCurdy-McKinnon D, Feusner JD. What happens after treatment? A systematic review of relapse, remission, and recovery in anorexia nervosa. J Eat Disord. 2017 Jun 14;5:20. doi: 10.1186/s40337-017-0145-3. PMID: 28630708; PMCID: PMC5470198.
- Prochaska, J. O., & DiClemente, C. C. (1983). Stages and processes of self-change of smoking: Toward an integrative model of change. Journal of Consulting and Clinical Psychology, 51(3), 390-395. http://doi.org/10.1037/0022-006X.51.3.390



